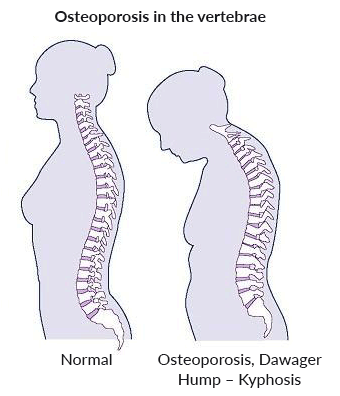
You might have heard this refrain: “I’m shrinking. I’m 2 inches shorter than I used to be. The older I get, the shorter I become!” The culprit most likely is osteoporosis, a bone disorder that reduces bone strength and bone density. It can lead to a forward curvature of the spine (hump), typically in women.
Besides causing spinal curvatures, osteoporosis is the underlying cause of most fractures in the elderly and postmenopausal women. It causes over 1.5 million fractures in the U.S. every year — most often vertebral fractures. This metabolic disease weakens the strength and quality of bone causing individuals to be more susceptible to unexpected fractures.
Some call it a silent disease since it usually progresses without pain or other symptoms. Often, the diagnosis is made post-fracture. According to the International Osteoporosis Foundation, 55% of the people over the age of 50 in the U.S. have osteoporosis or low bone mass. It’s a major health problem.
Fractures can occur in any bone but most broken bones in the above population occur in the spine, wrist and hip. Fifty percent of white women over the age of 50 will succumb to a fracture during their lifetime and white women get fractures 4 times more frequently than men.
Bone Basics
Bone is living tissue and a combination of collagen and calcium. Collagen provides bone with a soft framework and calcium phosphate gives it strength. About 1 percent of the body’s calcium is found in blood. The remaining 99 percent is contained in bone and teeth.
Trabecular bone looks like a sponge and its calcium crystals are found on the inside of healthy bones. It has a rich supply of blood vessels and is a source of calcium when blood calcium is low. Calcium is redeposited in this bone when the diet is plentiful with calcium.
Cortical bone is the hard, ivory, outer bone that wraps around the spongy trabecular bone. It forms the shaft of long bones. It fluctuates much less compared to trabecular bone.

Source Stock Photo Getty Images
Osteoporosis devitalizes bone, in particular, spongy bone. The holes in the “sponge” become larger and increase in number causing the inside of the bone to become weak, thin and fragile.
The body needs among other things, the minerals calcium and phosphorus to make and maintain strong, healthy bones. Bone is living tissue and the manufacturing of it is a dynamic process.
Bones remain healthy and strong as long as there is a good balance between new bone formation and old bone removal…
Throughout our lifetime, old bone is continuously removed (bone resorption) and continuously replaced by new bone (bone formation). Osteoclasts are bone-removing cells and osteoblasts are bone forming-cells.
During childhood and the teenage years, new bone is added to the skeleton faster than old bone is removed or resorbed. This is the period of greatest gain in bone density.
Starting in midlife, there’s a gradual decline in bone density for both men and women, but more pronounced for women. By age 65 and throughout life thereafter, men and women tend to lose bone tissue at the same rate. The problem at this time in their lives is that the body does not make enough new bone to counterbalance the greater amount of old bone that it reabsorbs causing a reduction in bone mass (osteopenia).
Source: U.S. Dept. of Health & Human services
What Causes Osteoporosis?
One can divide the reasons for this condition into primary and secondary risk factors.
Primary Unchangeable Risk factors
- Family history of osteoporosis or fractures
- Ethnicity — White and Asian women are at highest risk
- Age — The older you are, the greater the risk of osteoporosis
- Body size — Small, thin women are at greater risk
- Gender — Women get osteoporosis more frequently than men.
- Hormones — Estrogen deficiency in women (premature menopause naturally occurred or secondary to surgery). Testosterone deficiency in men.
- Genetic disorders
Secondary Changeable Risk Factors
- Medications — Certain medications, such as prednisone
- Exercise — Lack of exercise or long term bed rest
- Smoking cigarettes
- Alcohol Abuse
- Diet lack — A diet low in calcium and vitamin D makes you more susceptible to osteoporosis
- Diet excess — A diet overly rich in sodium, protein and caffeine
- Illness — many conditions, for example; illnesses with absorption problems, inflammatory bowel disease, bulimia, anorexia nervosa, diabetes chronic liver disease
Symptoms
Although some call it a silent disease, it can cause a severe backache, spontaneous fracture, collapse of a vertebra and loss of height is common.
The diagnosis not infrequently is made post-fracture, when image studies including a bone density test are performed which often reveal reduced bone mass. This test measures the amount of calcium in your spine and hips to check your bone strength and gauge whether the treatments are working to improve bone density.
Prevention and Treatment
Ideally, osteoporosis should be prevented since treatment can only partially reverse it. There are steps you can take to help keep your bones healthy and slow down bone loss:
- Eat a diet rich in calcium and vitamin D; consider supplements
- Exercise: Weight-bearing and muscle strengthening exercises
- Do not drink alcohol in excess
- Don’t smoke.
- Medication: Consult your physician about the side effects of medications prescribed to strengthen your bones.
- Take measures to prevent falling
Osteoporosis is the most common metabolic bone disease in the United States. It saps the life out of bones making them weak and brittle causing hundreds of thousands of fractures every year, especially among the elderly.
There are steps you can take to fight this disease and the earlier you start the better the results. Work with your doctor about treatment choices and be aware of the side effects of the suggested medications
References
- CDC; Does Osteoporosis Run in Your Family; May 13, 2018
- NIH; National Institute of Arthritis and Musculoskeletal and Skin Diseases; Osteoporosis; Feb 28, 2016
- National Osteoporosis Foundation — Osteoporosis
- Black DM, Rosen CJ; Postmenopausal Osteoporosis; N Engl J Med, Jan 21, 2016
This article is intended solely as a learning experience. Please consult your physician for diagnostic and treatment options.
